Maxillofacial surgery is a medical specialty that combines science, precision and aesthetics to treat disorders affecting the mouth, jaw, face and neck. Its aim is not only to correct a visible problem, but also to restore chewing function, improve breathing, balance the bite and restore facial harmony.
Unlike conventional dental surgery, maxillofacial surgeons work on deeper structures: bones, muscles, joints and soft tissues. Thanks to advances in 3D digital planning, surgical guides and minimally invasive surgery, today’s treatments offer pinpoint accuracy and faster recovery times.
It is common to resort to this speciality in cases of:
>>> Do you live in Mallorca? Book your free first appointment <<<
- Malocclusions or bite abnormalities, such as a receding jaw or prognathism.
- Complex extraction of wisdom teeth or jaw cysts.
- Orthognathic surgery to improve both facial function and aesthetics.
- Facial trauma, tumours or congenital defects.
Beyond physical appearance, maxillofacial surgery has a profound impact on self-esteem, oral health, and quality of life. A well-planned treatment can transform the way a person eats, breathes, and sees themselves.
Facial balance is achieved not only by correcting the shape, but also by restoring function. Maxillofacial surgery treats health and beauty as a whole.
When is maxillofacial surgery indicated?
Maxillofacial surgery is indicated when there are functional, aesthetic, or structural alterations that cannot be resolved through conventional dental treatments. Its scope of application is broad: from complex wisdom tooth extraction to the correction of facial deformities that affect bite, breathing, or facial expression.
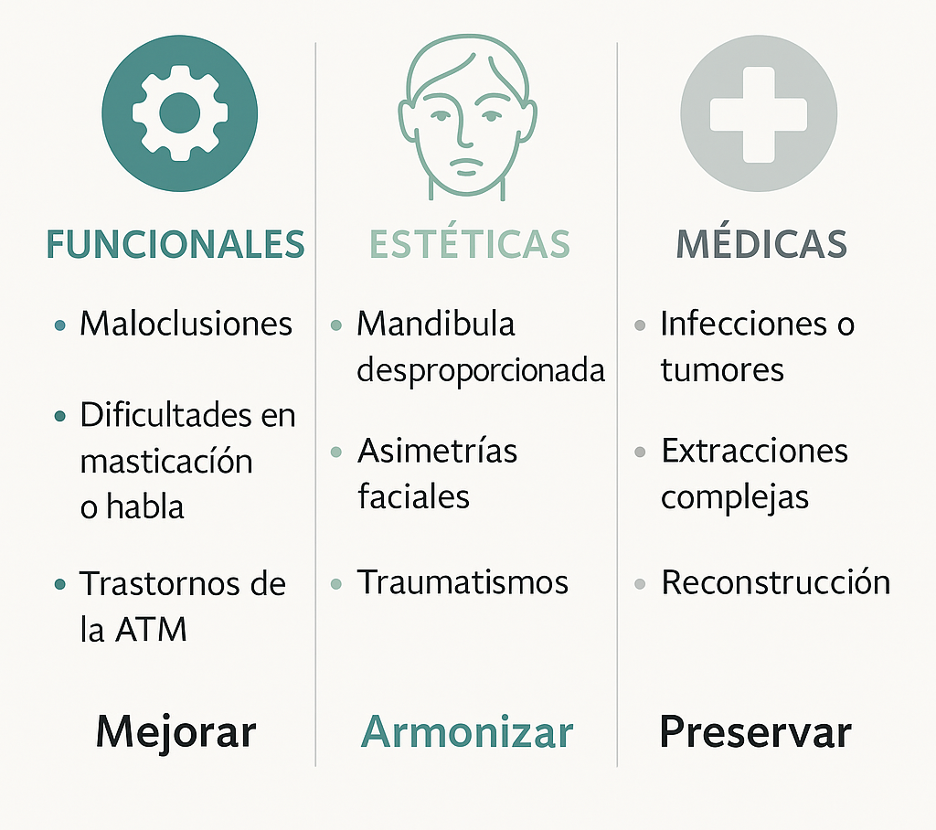
In general, the specialist evaluates three main groups of indications:
- Functional indications
These relate to chewing, swallowing, breathing or phonation. They include:
- Severe malocclusions or mandibular asymmetries.
- Difficulty chewing or speaking properly.
- Temporomandibular joint disorders (TMJ).
- Sleep apnoea due to mandibular retrusion.
- Aesthetic indications
These arise when a structural alteration affects facial harmony. Examples:
- Disproportionate jaw or chin.
- Facial asymmetries.
- After-effects of trauma or previous procedures. In these cases, maxillofacial surgery not only improves appearance, but also restores the balance between form and function.
- Medical indications
These include conditions that compromise oral or general health:
- Deep infections, cysts, or jaw tumours.
- Reconstruction following fractures or bone resections.
- Complex extractions, such as impacted wisdom teeth or teeth close to the dental nerve.
An accurate diagnosis allows us to determine whether the treatment will be reconstructive, orthognathic, oncological or implantological. The initial assessment usually includes panoramic X-rays, 3D CT scans and digital planning.
Table: type of problem and most appropriate maxillofacial treatment
Type of problem | Clinical example | Maxillofacial treatment indicated | Main objective |
Severe malocclusion or open bite | Prognathism, retrognathism, mandibular asymmetry | Bimaxillary orthognathic surgery | Improve bite and facial aesthetics |
Joint pain or jaw locking | TMJ disorder | Arthroscopy or arthrocentesis | Regain mobility and reduce pain |
Complex tooth extraction | Wisdom teeth included or close to the nerve | Controlled oral surgery | Prevent nerve damage or infection |
Facial trauma | Fractures of the jaw, cheekbone or eye socket | Reconstructive surgery with titanium plates | Restoring function and symmetry |
Maxillary tumours or cysts | Benign or malignant lesions | Surgical resection and reconstruction | Eliminate the pathology and preserve the bone |
Cosmetic alterations | Small chin, facial disproportion | Chin surgery or cosmetic orthognathic surgery | Harmonise the face and improve the profile |

Types of maxillofacial surgery
Maxillofacial surgery encompasses a wide range of procedures that act on the bones of the face, the oral cavity, and the masticatory system. Each procedure has a different objective, but all seek to restore function, eliminate pathologies, and improve facial harmony.
Orthognathic surgery
Corrects discrepancies between the upper and lower jaws that affect bite, breathing, or facial aesthetics.
- Indicated in cases of open bite, prognathism, or retrognathism.
- It uses 3D digital planning to guide bone cuts and predict results.
- Simultaneously improves chewing function and facial harmony.
Wisdom tooth surgery and complex extractions
Recommended when teeth are impacted, poorly positioned, or close to the dental nerve.
- It helps prevent infections, cysts, or tooth displacement.
- It is usually performed under local anaesthesia or conscious sedation.
- In complex cases, the surgeon evaluates the nerve relationship using 3D CT scans.
Reconstructive and post-traumatic maxilofacial surgery
Aimed at restoring bone and soft tissue following fractures, accidents or tumour resections.
- It uses titanium plates, bone grafts, or resorbable meshes.
- In severe cases, customised 3D printing is planned.
- Its objective is to restore facial symmetry and joint function.
Implant and regenerative maxilofacial surgery
Enables complex dental implants to be fitted or lost bone to be regenerated.
- It includes techniques such as bone grafts, maxillary sinus elevation, and guided regeneration.
- Indicated in patients with bone loss or previous failed treatments.
Oncological and salivary gland surgery
This includes the removal of cysts, benign or malignant tumours, and glandular disorders.
- It focuses on removing pathological tissue while preserving vital structures.
- It can be combined with immediate reconstruction to minimise aesthetic sequelae.
Complementary facial maxilofacial cosmetic surgery
Includes procedures that harmonise the face and complement functional treatments.
- Chin augmentation, rhinoplasty, buccal fat removal, or facial lipostructure.
- It provides balance and proportion, improving the overall perception of the face.
Comparison table: types of maxillofacial surgery, purpose, recovery and results
Type of surgery | Main purpose | Recovery time | Expected results |
Orthognathic | Correcting bite and facial symmetry | 3–6 weeks | Improved function and aesthetics |
Wisdom tooth extraction | Avoid infections or displacements | 3–7 days | Rapid recovery with no after-effects |
Reconstructive | Repair damaged bones or tissues | 4–8 weeks | Restore function and symmetry |
Implantology | Replacing teeth and regenerating bone | 2–4 weeks | Stability and dental aesthetics |
Oncology | Remove lesions or tumours | Variable | Disease control |
Facial aesthetics | Improve facial proportions | 1–3 weeks | Facial harmony and confidence |
Modern maxillofacial surgeries are not only safer, but are also supported by digital planning and advanced biomaterials, allowing each procedure to be customised and achieving natural and predictable results.
Orthognathic surgery: restoring balance between facial function and aesthetics
Orthognathic surgery is one of the most representative procedures in modern maxillofacial surgery. Its objective is to reposition the jaws to correct bite abnormalities, improve breathing, and balance facial proportions. Although it is often associated with aesthetic purposes, its functional impact is equally or even more important.
It is indicated in patients with problems such as:
- Open bite or crossbite, where the teeth do not fit together properly.
- Mandibular prognathism or retrognathism, with an advanced or receding jaw.
- Facial asymmetries that affect the balance of the face.
- Respiratory or sleep disorders, especially in cases of obstructive apnoea.
Orthognathic surgery combines technological precision and interdisciplinary planning between the maxillofacial surgeon and the orthodontist. Currently, procedures are designed using 3D digital models, which allow the final result to be predicted in terms of both occlusion and facial expression.
Stages of orthognathic treatment
Process stage | What is done | Professionals involved | Approximate duration |
Initial diagnosis | Photographic study, cephalometric analysis and 3D scan | Orthodontist and maxillofacial surgeon | 1–2 weeks |
Digital planning | Simulation of jaw movements and occlusion | Maxillofacial surgeon | 2–3 weeks |
Previous orthodontic treatment | Teeth alignment before surgery | Orthodontist | 6–18 months |
Surgical procedure | Maxillary and/or mandibular repositioning under general anaesthesia | Maxillofacial surgeon | 2–4 hours |
Recovery and control | Post-operative check-up and orthodontic refinement | Interdisciplinary team | 3–6 months |
Expected results
- Functional: improved bite, chewing, speech and breathing.
- Aesthetic: facial balance, more harmonious profile and relaxed expression.
- Psychological: increased self-esteem and improved self-image.
Recovery usually takes between 3 and 6 weeks, depending on the type of bone movement. During this time, a soft diet, thorough hygiene and regular check-ups with the medical team are recommended.
Orthognathic surgery does not seek to change the face, but rather to harmonise it with its natural structure, restoring lost functionality and the patient’s confidence.
Risks, recovery, and post-operative care
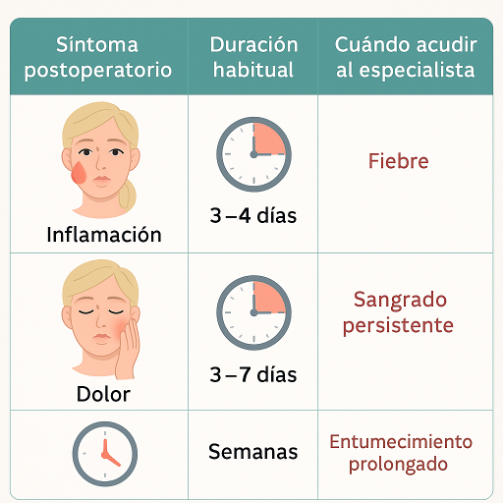
All maxillofacial surgery, no matter how advanced, requires a supervised recovery process and proper post-operative care. Although the results are usually excellent, it is essential to be aware of the possible side effects, risks and recovery times to ensure a favourable outcome.
Most common risks and complications
In most cases, discomfort is temporary and can be controlled with medication. However, it is important to be aware of the possible effects depending on the type of surgery:
Complication | Common cause | Estimated duration | Medical recommendation |
Facial swelling | Normal reaction to surgical trauma | 3–7 days | Apply cold locally, keep head elevated |
Pain or tenderness | Tissue or nerve irritation | 3–10 days | Painkillers and relative rest |
Bruises or haematomas | Capillary fragility or bone manipulation | 7–15 days | Do not massage, avoid exposure to sunlight. |
Light bleeding | In oral surgery or wisdom tooth surgery | 24–48 hours | Compression with sterile gauze |
Postoperative infection | Poor hygiene and tobacco | Rare (less than 5%) | Antibiotics and medical supervision |
Temporary sensory disturbance | Irritation of the dental or mental nerve | Weeks or months | Neurological monitoring and physiotherapy if necessary |
In the hands of an experienced maxillofacial surgeon, serious complications are rare. The key lies in preoperative planning and strictly following the specialist’s guidelines.
Essential care during recovery
- Keep the area clean and dry, using mild rinses with chlorhexidine or saline solution.
- Avoid tobacco and alcohol, as they delay healing.
- Sleep with your head slightly elevated to reduce inflammation.
- Follow a bland, cold diet for the first few days (purees, yoghurts, creams, warm soups).
- Do not engage in strenuous physical activity for at least 15 days.
- Monitor medication according to the specialist’s guidelines (painkillers, antibiotics, anti-inflammatories).
- Attend check-ups to remove stitches or assess progress.
The time required for full recovery varies: from one week for minor surgery to six weeks for orthognathic or reconstructive procedures.
The success of maxillofacial surgery does not end in the operating theatre, but rather in the care that the patient maintains afterwards. Consistency and hygiene are the best complement to surgical technique.
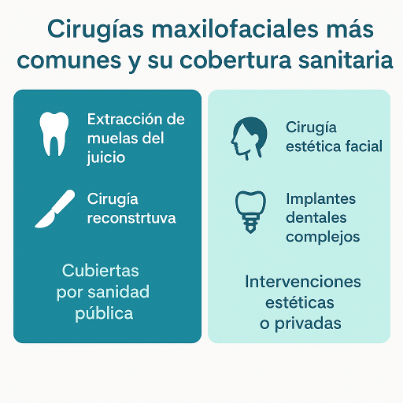
Prices and financing for maxillofacial surgery
The cost of maxillofacial surgery can vary widely depending on the type of procedure, the complexity of the case, the technology used, and the experience of the surgical team. Although price is an important factor, it must be understood within a medical context: the essential thing is to ensure safety, precision, and long-term functional and aesthetic results.
Factors influencing price
Variable | How it affects the cost | Estimated range |
Type of surgery | Simple procedures (such as wisdom teeth removal) are more affordable than orthognathic or reconstructive surgery. | From €250 to over €8,000 |
Complexity of the case | Patients with severe asymmetries, fractures, or bone loss require advanced planning and more surgical time. | +20–40 per cent on the base price |
Type of anaesthesia | Local, conscious sedation or general anaesthesia (requires hospital operating theatre). | 80 €–1.000 € |
Hospital or clinic | Centres with 3D technology and multidisciplinary teams tend to be more expensive, but they also offer better results and lower risk. | Variable |
Maxillofacial surgeon | The professional’s experience and expertise directly influence the cost and predictability of the outcome. | Variable |
Coverage or funding | Some treatments may be covered by Social Security or medical insurance, especially functional treatments. | Partial or total, depending on the case |
Indicative price examples
Type of procedure | Approximate price in a private clinic (Spain) | Public health coverage |
Wisdom tooth extraction | 150 € – 300 € | Yes, if medically indicated. |
Orthognathic surgery | 6.000 € – 9.000 € | Partial in functional cases |
Facial reconstructive surgery | 4.000 € – 10.000 € | Yes, depending on the pathology |
Complex dental implants | 1.000 € – 2.500 € | No |
Facial cosmetic surgery (chin augmentation, functional rhinoplasty, etc.) | 2.000 € – 6.000 € | No |
Salivary gland surgery or tumours | 3.000 € – 7.000 € | Yes, full coverage |
The prices indicated are approximate and may vary depending on the city, clinic, and individual needs of the patient.
Financing and payment facilities
Most maxillofacial clinics offer personalised financing plans, allowing you to pay for treatment in interest-free monthly instalments during the first few months. In addition, some private health insurance policies cover functional or oncological procedures, although not cosmetic procedures.
Practical advice: it is always advisable to request a detailed quote with a breakdown of medical fees, anaesthesia, surgical materials and post-operative follow-up, to avoid hidden costs.
Un tratamiento maxilofacial debe considerarse una inversión en salud, función y confianza. Los resultados bien planificados tienen un valor que trasciende el precio.
Long-term results and benefits
Maxillofacial surgery offers much more than just aesthetic improvement. Its benefits are reflected in the patient’s function, health and quality of life, providing stable and long-lasting results. Thanks to advances in digital planning and minimally invasive techniques, the changes are predictable, natural and progressive.
Functional benefits
- Improved chewing and digestion, by correcting bite problems or jaw asymmetry.
- Greater respiratory comfort, especially after orthognathic or reconstructive surgery.
- Relief of pain and muscle tension in cases of temporomandibular joint (TMJ) dysfunction.
- Improved pronunciation and phonation, by rebalancing the relationship between the lips, tongue and jaw.
Aesthetic benefits
- A more symmetrical and balanced face, with natural and consistent proportions.
- Harmonious profile and relaxed expression, the result of profound structural correction.
- Indirect facial rejuvenation, thanks to bone and soft tissue restoration.
- Long-lasting results, without the need for frequent touch-ups.
Psychological and social benefits
- Increased self-esteem and confidence in personal image.
- Reduction in social anxiety and improvement in emotional wellbeing.
- Greater satisfaction with overall health and appearance.
Long-term success depends on clinical follow-up and maintaining good oral hygiene, healthy habits and regular check-ups. In most patients, the functional and aesthetic benefits last a lifetime.
The true success of maxillofacial surgery is measured when the patient can smile, eat and express themselves without limitations once again. Aesthetics are only the visible consequence of having regained function.
Maxillofacial surgery as a balance between health, function and facial harmony
Maxillofacial surgery is one of the most comprehensive medical disciplines, integrating oral health, facial reconstruction and aesthetics into a single field. Its purpose goes far beyond improving appearance: it seeks to restore the natural function of the face, returning the ability to chew, breathe, speak and smile normally.
Thanks to the combination of 3D technology, minimally invasive techniques and personalised planning, it is now possible to achieve results that respect the patient’s identity while improving their physical and emotional well-being. Every procedure, from wisdom tooth extraction to complete orthognathic surgery, follows the same philosophy: balancing form and function.
Seeing a qualified maxillofacial surgeon ensures a comprehensive diagnosis and a safe treatment plan. This specialist works not only on the teeth or bones, but on the overall structure of the face, ensuring that each procedure is consistent with the patient’s anatomy, expression and expectations.
Maxillofacial surgery does not seek to change who you are, but rather to restore harmony to your face and functionality to your life.
Frequently asked questions about maxillofacial surgery
Maxillofacial surgery raises many questions, especially in patients undergoing facial surgery for the first time. Below are the most common questions with clear, medically verified and easy-to-understand answers.
How much does maxillofacial surgery cost?
The price depends on the type of procedure, its complexity, and the centre where it is performed. In Spain, simple surgeries such as wisdom tooth extraction cost around €150–300, while orthognathic or reconstructive surgery can exceed €6,000–9,000. In the public health system, functional procedures are usually covered in full or in part.
Does maxillofacial surgery hurt?
Thanks to local or general anaesthesia, you will not feel any pain during the procedure. After the operation, you may experience moderate discomfort, which can be controlled with painkillers and anti-inflammatory medication. The discomfort usually subsides within a few days.
How long does recovery take?
It depends on the type of surgery: from one week for simple extractions to six weeks or more for orthognathic or reconstructive procedures. The patient can gradually return to their routine following medical guidelines.
What are the main risks?
As with any surgery, there are minimal risks: infection, inflammation, minor bleeding, or temporary numbness. These effects are temporary and rare if the procedure is performed by a qualified specialist.
What is the difference between maxillofacial surgery and cosmetic surgery?
Maxillofacial surgery has a functional and medical objective (correcting bite, breathing or injuries), while cosmetic surgery seeks to improve appearance. In many cases, the two complement each other to achieve a natural balance between health and facial harmony.
Who can undergo orthognathic surgery?
It is indicated for patients with complete bone growth, generally from the age of 18 onwards, who have bite problems, asymmetries or respiratory disorders. It requires a joint assessment by an orthodontist and a maxillofacial surgeon.
Is the change very noticeable after surgery?
The result is usually harmonious and natural, as the procedure respects facial proportions. It does not transform the face, but rather restores the patient’s original symmetry and expression.
Can I finance the treatment?
Yes. Most clinics offer interest-free financing plans for several months, as well as facilities for combined treatments with orthodontics or implantology.
Is it a safe surgery?
Yes. Thanks to 3D digital technology and meticulous planning, modern maxillofacial surgery is very safe and predictable, with success rates exceeding 95%.
When should I see a maxillofacial surgeon?
When there are problems with bite, jaw pain, difficulty chewing, breathing or swallowing, or visible facial alterations. They are also the appropriate specialist for cases of trauma, tumours or jaw cysts.
 Whatsapp
Whatsapp



