Sialorrhea, also known as ptyalism, is a condition characterised by excessive saliva production or difficulty controlling it in the mouth. Although it is usually associated with young children or certain neurological conditions, it can also occur in adults, especially when there is an imbalance between the amount of saliva produced and the ability to swallow it.
Under normal conditions, the salivary glands (parotid, submandibular, and sublingual) produce around 1 to 1.5 litres of saliva per day. This fluid performs essential functions: it keeps the mucosa hydrated, facilitates swallowing, initiates digestion, and protects the teeth from bacteria. When production increases or neuromuscular control is altered, saliva accumulates or overflows, causing both physical and social discomfort.
Sialorrhea can be:
>>> Do you live in Mallorca? Book your free first appointment <<<
- Physiological, as occurs in babies or during teething, without pathological implications.
- Pathological, when it appears in adults or persists in older children, usually associated with neurological diseases, side effects of medications, or oral disorders.
Beyond aesthetic discomfort, this condition can affect the patient’s communication, eating habits, and self-esteem, and therefore warrants medical attention and specialised treatment.
Type of sialorrhea | Main cause | Clinical characteristics | Common example |
Physiological | Normal stimulation of salivary glands (babies, teething) | Transient, without underlying disease | Infants aged 3 to 18 months |
Pathological | Neurological or mechanical impairment | Excess saliva that leaks from the corners of the mouth or accumulates in the oral cavity. | Parkinson’s disease, ALS, poorly fitted prostheses |
Pharmacological | Adverse effect of certain medicines | Increased salivary secretion after starting treatment | Clozapine, pilocarpine, morphine |
Situational or temporary | Hormonal changes, stress, reflux, or pregnancy | Mild and temporary hypersalivation, improves when the causal factor is corrected. | Pregnancy or acute anxiety |

Main causes of excessive salivation
Sialorrhea is not a disease in itself, but rather a clinical symptom that can have multiple causes. In some cases, there is actual hyperproduction of saliva, but often the problem lies in an alteration of motor control or swallowing. Correctly identifying the origin is essential for choosing the appropriate treatment.
Table: causes of sialorrhea, mechanism and therapeutic approach
Category | Specific cause | Pathophysiological mechanism | Guidance-oriented therapeutic approach |
Neurological | Parkinson’s disease, cerebral palsy, ALS, stroke | Difficulty coordinating oral and swallowing muscles; reduced swallowing reflex | Orofacial rehabilitation, physiotherapy, botulinum toxin in salivary glands |
Pharmacological | Clozapine, pilocarpine, morphine, lithium | Stimulation of muscarinic receptors → increased salivary secretion | Adjustment or change of medication, anticholinergic treatment (glycopyrrolate, scopolamine) |
Oral the place | Oral infections, poorly fitting dentures, mouth ulcers or gum irritation | Reflex stimulation of salivary glands due to inflammation or mechanical trauma | Dental treatment, denture adjustment, anti-inflammatory mouthwashes |
Endocrine or physiological | Pregnancy, gastroesophageal reflux, anxiety or stress | Hormonal or autonomic changes that increase secretion | Management of the underlying cause, hygiene and dietary measures |
Toxic or infectious | Poisoning by mercury, organophosphate insecticides, or systemic infections | Intense parasympathetic stimulation of the glands | Emergency treatment and detoxification |
Postural or mechanical | Mandibular abnormalities, macroglossia, weak lips | Difficulty retaining or directing saliva within the mouth | Speech therapy exercises, kinesiotape, postural re-education |
In adults, neurological and pharmacological causes are the most common, while in children, the neuromotor or postural form predominates. The correct diagnosis should include neurological assessment and review of current medication, as both factors often coexist.
Types and clinical classification of sialorrhea
From a medical point of view, sialorrhea can be classified according to its origin, location, or duration. This classification is essential for guiding diagnosis, as not all types of sialorrhea respond equally to treatment.
Comparative table: types of sialorrhea and clinical characteristics
Type of sialorrhea | Description | Location of excess saliva | Clinical consequences | Typical example |
Previous | Saliva spills out through the corners of the mouth. | Mouth → lips → chin | Perioral skin irritation, unpleasant odour, aesthetic impact. | Patients with Parkinson’s disease or facial paralysis. |
Rear | Saliva accumulates in the oropharynx and may be swallowed or aspirated. | Mouth → throat → airway | Coughing, choking, risk of pulmonary aspiration. | Patients with ALS or bulbar lesions. |
Chronicle | Persistent for more than three months. | Variable depending on the case. | It interferes with eating, speaking and self-esteem. | Hypersalivation due to established neurological injury. |
Acute or transient | Short-lived, associated with irritation, infections, or pregnancy. | Located. | It disappears when the cause is treated. | Excessive salivation due to mouth ulcers, reflux or pregnancy. |
Physiological | Excessive saliva in normal situations. | Widespread. | No treatment required. | Infants or teething. |
Pathological | Excess due to neurological, pharmacological or anatomical causes. | Variable. | He needs medical or speech therapy intervention. | Parkinson’s disease, clozapine, macroglossia. |
Difference between sialorrhea and ptyalism
Term | Definition | Key difference |
Sialorrhea | Excessive saliva flow due to difficulty controlling or swallowing it. | It may be due to either hypersalivation or motor problems. |
Ptialism | Actual increase in salivary secretion. | It always involves excessive production, not a control problem. |
In medical practice, the term sialorrhea encompasses both mechanisms—hyperproduction and poor neuromotor control—but differentiating between the two helps to determine whether treatment should be pharmacological (reducing secretion) or rehabilitative (improving swallowing).
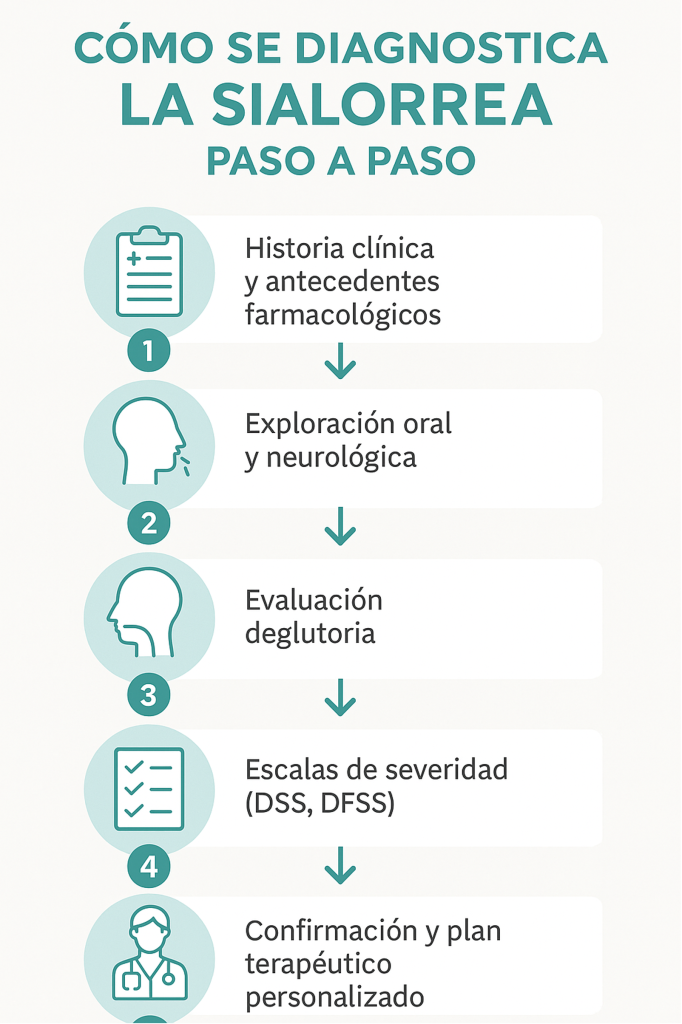
Diagnosis and medical evaluation of sialorrhea
The diagnosis of sialorrhea requires determining whether the problem is due to excess production or difficulty in controlling and swallowing saliva. To do this, a comprehensive assessment is carried out that combines a physical examination, analysis of medical history, and additional tests.
The diagnostic process seeks to answer three key questions:
- Is too much saliva being produced?
- Is there a motor or neurological disorder that prevents you from controlling it?
- What impact does it have on the patient’s quality of life?
Table: main diagnostic methods and their purpose
Assessment method | Clinical objective | What information does it provide? |
Complete medical history | Identify possible medical or pharmacological causes. | Temporary relationship with neurological diseases, pregnancy, or drugs (e.g., clozapine). |
Oral and dental examination | Assess the anatomy and condition of the prostheses or mucous membranes. | Detects local irritation, infections, or poor prosthetic fit. |
Neurological and motor assessment | Analyse the coordination of oral muscles and swallowing reflex. | Determine whether there is motor dysfunction, as in Parkinson’s disease or ALS. |
Clinical scales (DSS, DFSS) | Measure the severity and frequency of drooling. | They enable the progress and effectiveness of treatment to be quantified. |
Imaging tests (ultrasound, MRI) | Examine the salivary glands. | Detects inflammation or glandular hypertrophy. |
Pharmacological study | Review current medications. | It allows the identification of drugs that stimulate salivary secretion. |
Clinical note: drooling severity scales, such as the Drooling Severity and Frequency Scale, help to standardise assessment and adjust treatment based on the social and physical impact on the patient.
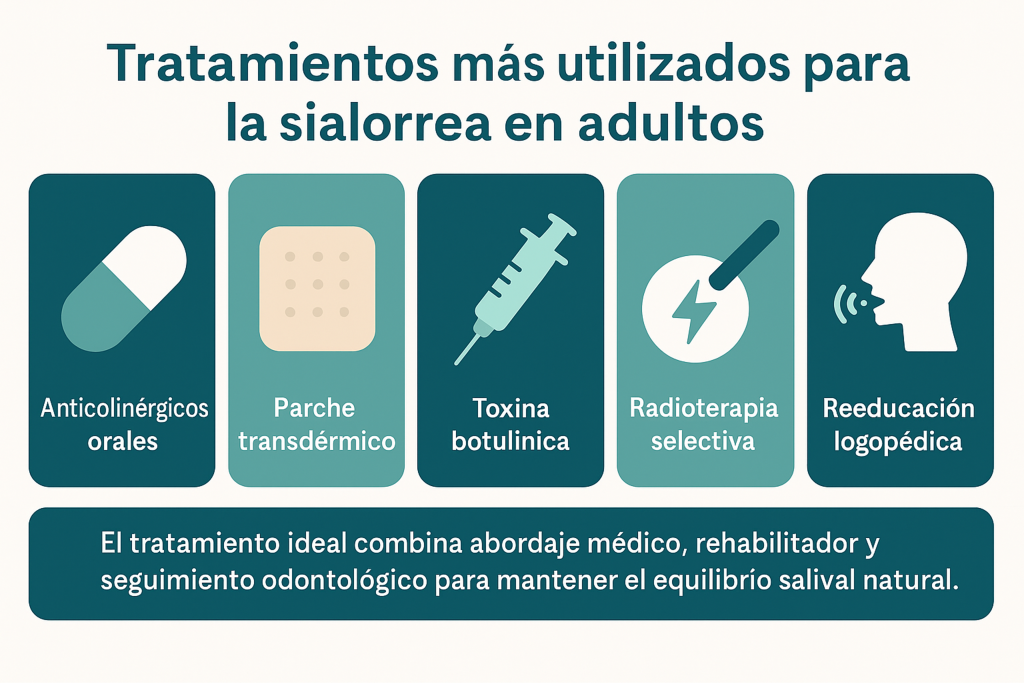
Medical and pharmacological treatment of sialorrhea
The management of hypersalivation depends on its cause, severity, and functional or social impact. In many cases, treatment combines medical, pharmacological, and rehabilitative measures to achieve a gradual and safe reduction in excess saliva. The aim is not to completely eliminate saliva production—which would be harmful—but to control it within physiological levels.
The approach should be multidisciplinary, involving dentists, neurologists, speech therapists, and orofacial physiotherapists.
Type of treatment | Mechanism of action | Clinical indications | Observations or side effects |
Oral anticholinergics (glycopyrrolate, scopolamine, atropine) | Block muscarinic receptors in salivary glands → reduce saliva production | Mild to moderate hypersalivation, especially in patients with Parkinson’s disease or ALS | Dry mouth, blurred vision, constipation; contraindicated in glaucoma and frail elderly patients. |
Scopolamine transdermal patch | Inhibits salivary secretion through progressive skin absorption. | Alternative in patients with poor oral compliance | May cause dizziness or drowsiness; the application area should be rotated. |
Botulinum toxin type A (BoNT-A) | Inhibits the release of acetylcholine in the parotid and submandibular glands. | Moderate or severe neurological hypersalivation | Temporary effect (3–6 months); requires ultrasound-guided infiltration |
Selective breast radiation therapy | Reduces the function of the salivary glands through targeted radiation. | Severe cases or cases resistant to pharmacological treatment | Risk of excessive dryness and permanent salivary hypofunction |
Selective surgery (ligation or resection of glands) | Permanent mechanical reduction of salivary flow | Severe cases with recurrent aspirations or failure of other treatments | Irreversible intervention, requires hospital assessment |
Speech therapy / orofacial physiotherapy | Neuromuscular retraining and improvement of tongue and jaw posture | Complementary in all phases of treatment | Improves swallowing and reduces dependence on medication |
Botulinum toxin type A is considered the treatment of choice in patients with Parkinson’s disease or ALS, as it achieves stable results and significantly improves quality of life without significant systemic effects. In mild cases, a combination of speech therapy and anticholinergic drugs is usually sufficient to control symptoms.
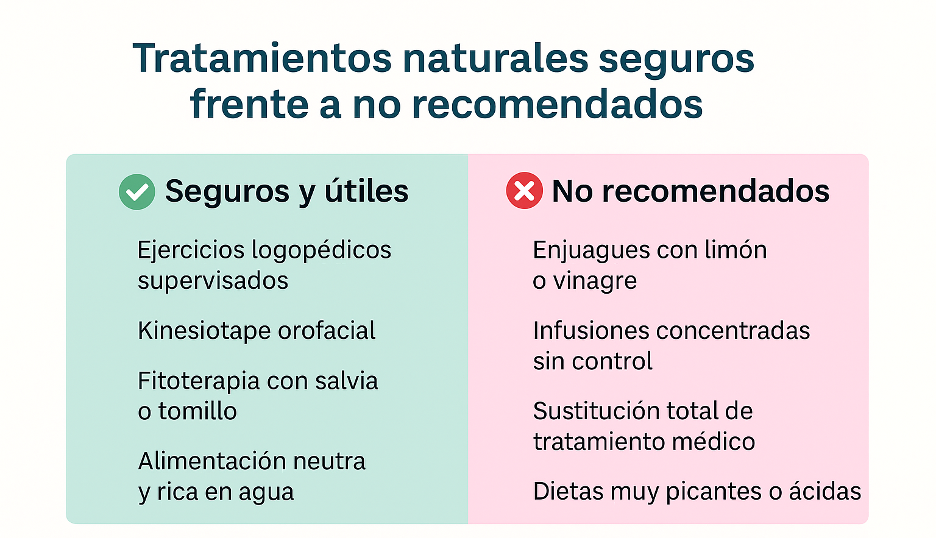
Natural and supportive treatments for excessive salivation
In addition to drugs and botulinum toxin, there are complementary strategies that help to reduce hypersalivation in a non-invasive way. These treatments are especially useful in patients with mild hypersalivation, in the early stages or as maintenance after medical therapy.
The aim is to improve muscle control, re-educate swallowing and reduce stimuli that increase salivary production, while maintaining the lubricating and protective function of saliva.
Tailored therapy | Main objective | Clinical evidence or efficacy | Observations |
Neuromuscular re-education and speech therapy | Training tongue control, swallowing and jaw posture | High in mild to moderate sialorrhea (complementary to other treatments) | Requires regular sessions with a specialist speech therapist. |
Orofacial kinesiotape | Stimulate proprioception and improve lip closure | Growing evidence in orofacial physiotherapy | It does not produce side effects if applied correctly. |
Postural and breathing exercises | Re-educate head position and breathing control | Moderate, improves swallowing in neurological patients | They must be prescribed by a specialist physiotherapist. |
Herbal medicine (sage, thyme, mint) | Reduce salivary secretion due to its mild anticholinergic effect. | Low to moderate; useful as natural support | It does not replace medical treatment. |
Enhanced oral hygiene | Reduce irritation and infections that increase salivation | High; essential for the success of any therapy | Use of mild, alcohol-free mouthwashes |
Avoid acidic or highly spiced foods. | Reduce excessive salivary stimulation | Practical evidence | General dietary recommendation |
Natural treatments are most effective when combined with speech therapy and orofacial physiotherapy. Their effect is not immediate, but they help maintain long-term salivary control stability and reduce the need for medication.
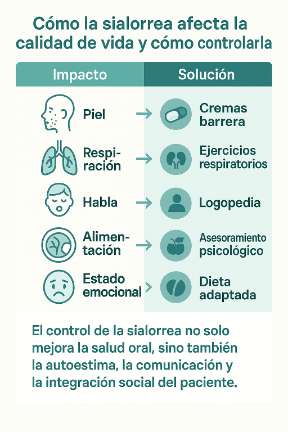
Complications and quality of life in patients with sialorrhea
Beyond aesthetic or social discomfort, hypersalivation can cause physical, respiratory, and emotional complications that significantly affect the patient’s daily life. Therefore, treatment should not be limited to reducing saliva production, but also to preventing the consequences of its persistence.
Type of complication | Common manifestations | Potential consequences | Preventive or therapeutic measures |
Dermatological | Irritation, erythema, and maceration of the skin around the mouth and neck | Skin infections, pain or unpleasant odour | Use barrier creams, keep the area dry and ventilated. |
Respiratory | Aspiration of saliva into the airways | Chronic cough, aspiration pneumonia | Postural and swallowing re-education, botulinum toxin, respiratory physiotherapy |
Oral and digestive | Alteration of oral pH, tooth decay, halitosis | Infections, gingivitis, or tooth loss | Enhanced oral hygiene, mild mouthwashes, regular dental check-ups |
Social and emotional | Isolation, anxiety, embarrassment, or difficulty speaking | Decreased self-esteem and emotional well-being | Psychological support, environmental education, comprehensive treatment |
Nutritional | Weight loss or difficulty feeding | Malnutrition in severe cases | Adapted diet and speech therapy assistance during feeding |
Final reflection: how to address excessive salivation holistically
Sialorrhea is a complex symptom that can affect both the physical health and quality of life of the patient. Although there is not always a definitive cure, it can be controlled through a multidisciplinary medical approach that combines accurate diagnosis, pharmacological or rehabilitative treatment, and personalised support measures.
The success of the treatment depends on three pillars:
- Identify the cause (neurological, pharmacological, postural, or physiological).
- Apply the appropriate treatment (from speech therapy to botulinum toxin or selective surgery).
- Maintain constant monitoring to adjust interventions according to the patient’s progress.
Patient and carer education is key: understanding the mechanisms that cause excess saliva and knowing how to manage it in daily life reduces complications, improves self-esteem and restores autonomy and well-being.
Clinical conclusion:
With proper diagnosis and personalised treatment, most cases of sialorrhea can improve significantly. The key is to not resign yourself to the symptom and seek specialised medical help as soon as possible.
Management stage | Recommended action | Professional involved | Clinical objective |
1. Initial assessment | Medical history, medication review, and neurological examination | Dentist, neurologist | Determine the root cause |
2. Functional diagnosis | Swallowing assessment, drooling scales, imaging tests | Speech therapist, physiotherapist | Quantify severity |
3. Medical or rehabilitative treatment | Anticholinergics, botulinum toxin, or intensive speech therapy | Specialist doctor, speech therapist | Control secretion and improve coordination |
4. Monitoring and adjustment | Quarterly or half-yearly review of therapeutic effect | Multidisciplinary team | Maintaining results and preventing complications |
5. Education and support | Hygiene tips, habits, and emotional support | Caregivers, psychologist | Promoting adherence and quality of life |
A comprehensive approach to sialorrhea combines medicine, rehabilitation, and patient education to achieve sustained control and a more comfortable life.
Frequently asked questions about excessive salivation
Below are the most common questions from patients and carers about sialorrhea, along with clear answers based on medical evidence. This format helps to quickly resolve doubts and improves understanding of treatments and their expectations.
FAQ
1. Is there a definitive cure for excessive salivation?
In most cases, sialorrhea can be effectively controlled, although it is not always completely eliminated. Speech therapy, anticholinergic drugs, and botulinum toxin type A can reduce saliva production and improve oral control. In severe or persistent cases, there are surgical options that offer lasting results.
2. Why does excessive salivation occur in Parkinson’s disease?
In Parkinson’s disease, saliva production is not higher than normal, but patients swallow less frequently per minute due to slow movements and muscle rigidity. This causes saliva to accumulate in the mouth and eventually leak out. Treatments aim to stimulate swallowing and reduce secretion.
3. What role does botulinum toxin play in the treatment of excessive salivation?
Botulinum toxin type A is considered the most effective and safest treatment for neurological hypersalivation. It is injected into the parotid and submandibular salivary glands, temporarily inhibiting the release of acetylcholine, which reduces saliva production for 3 to 6 months.
4. Can excessive salivation be treated during pregnancy?
Yes. During pregnancy, excessive salivation is usually caused by hormonal and digestive changes and tends to improve after the first trimester. It is recommended to stay well hydrated, chew xylitol gum, and drink mild sage or mint tea, avoiding medication except in severe cases.
5. What foods or habits worsen excessive salivation?
Acidic, spicy, or highly seasoned foods stimulate the salivary glands and can worsen symptoms. Stress, tobacco, and certain medications such as clozapine or pilocarpine also increase salivary secretion. Controlling these factors helps improve the condition.
6. How can excessive salivation be reduced naturally?
The most effective natural options are speech therapy (to improve tongue control and swallowing) and orofacial kinesiotaping, which promotes lip closure. Infusions of sage, thyme or mint can complement the treatment, but should never replace medical intervention.
7. What is the difference between sialorrhea and ptyalism?
Sialorrhea can be caused by either excessive production or poor management of saliva within the mouth. Ptyalism, on the other hand, involves an actual increase in salivary secretion, without neuromotor alteration. In clinical practice, both terms are used similarly, although they are not identical.
8. Can excessive salivation cause respiratory infections?
Yes. When saliva accumulates and goes unnoticed in the airways, it can cause chronic coughing, bronchoaspiration, or aspiration pneumonia. It is important to monitor body position and perform swallowing exercises to reduce this risk.
9. Which specialists treat excessive salivation?
It depends on the cause. Treatment usually involves dentists, neurologists, speech therapists, orofacial physiotherapists, and ENT specialists. The most effective treatment is achieved through a coordinated approach between these specialists.
10. What happens if hypersalivation is not treated?
If left untreated, hypersalivation can cause skin irritation, halitosis, feeding problems, and social isolation. In severe cases, it also increases the risk of lung infections and malnutrition. It is therefore recommended to see a specialist as soon as symptoms persist for more than two weeks.
 Whatsapp
Whatsapp

